G Point PRP
G Point PRP
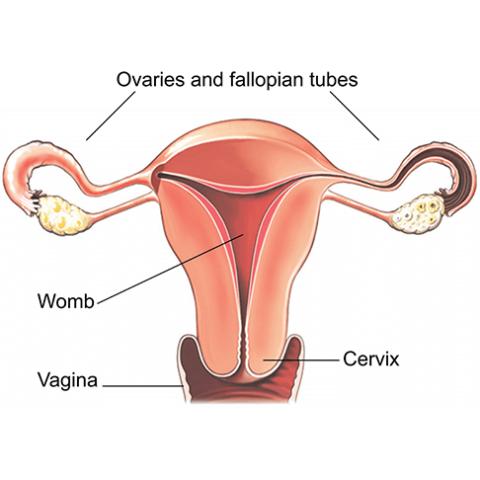
The G-Spot Shot is an injection of Platelet-Rich Plasma (PRP) delivered into the clitoral and vaginal areas. The PRP is derived from the patient’s blood. Getting a G-Spot Shot stimulates blood flow and cell growth, increasing sensitivity during sex.
The G-Spot Shot can treat numerous problems, such as decreased sensitivity, urinary incontinence, vaginal dryness, and sexual dysfunction.
Ideal G-Spot Shot candidates are women who want to improve their sexual health. women who are suffering from vaginal dryness, pain in the pelvic floor, urinary incontinence, and diminished sexual pleasure can be good candidates.
The G-Spot Shot can also be beneficial for menopausal and post-menopausal women. You may be a good candidate if you are seeking an increase in sexual desire and have realistic expectations about the procedure.